Blood Gas Analysis (BGA) is almost a routine test in patients admitted in ICCU/ICU.
Recently, I visited a relative admitted to the ICCU of a medical institute and there, I found the consultant doctors discussing the accuracy of BGA reports. Their conclusion was that most of the time the results were not satisfactory.
Unfortunately, a month ago, I was admitted to the same institute for my renal calculi surgery and due to some post-operative complications, I was shifted to the ICU. At the ICU,
My BGA was done thrice and to my dismay, all three times the residents collecting my blood from the radial artery were unaware of the proper heparin to blood ratio.
Then, I realized why the reports of BGA were not satisfactory. This prompted me to write this letter about sampling and the choice of blood for BGA.
Blood Sampling:
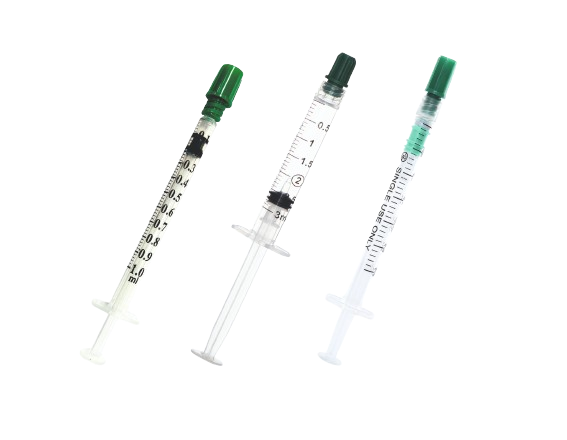
Heparinised blood is used for BGA, but the correct amount of heparin and blood is crucial to prevent coagulation and to obtain accurate test results. It has been recommended by the International Federation of Clinical Chemistry (IFCC) that heparin should be taken in the syringe to lubricate the inner wall of the syringe and then heparin should be expelled from the syringe entirely and at least 20 times the dead space volume of blood should be collected [1]. The dead space of the syringe is the volume of liquid remaining in the hub and the needle after completely emptying the syringe. It varies with the size of the syringe and the needle, type of material, etc. On average, the dead space is 0.08–0.25ml depending on the size of the syringe and needle (1ml-10ml). So as per IFCC recommendations, if we collect blood in a 2ml heparinised syringe, then considering the dead space about 0.1ml, the syringe should be completely filled (2ml) to make the blood 20 times the dead space volume. Under-filling the syringe would result in incorrect results due to dilution and chemical effects. The dilution effect of heparin may cause a fall in pCO2 and bicarbonate concentration, and since the heparin is acidic, the use of concentrated heparin may result in an increase in pCO2 and reduction in pH. pO2 may also be influenced by too much heparin. This problem of dilution effects of heparin can be avoided by using a syringe pre-loaded with lyophilized heparin, but under-filling of this syringe would also result in inaccurate results. Moreover, such syringes are costly. It is also preferred to use low concentration heparin (1000IU/ml) because this would result in a Final Heparin Concentration (FHC) of about 50IU/ml in a fully filled 2ml syringe, which would be sufficient for accurate BGA results. However, the heparin used in our hospitals for anti-coagulation treatment of patients is usually 5000IU/ml, and the same is generally used for heparinising the syringe for blood collection. This heparin would result in higher FHC (e.g., 250IU/ml in a fully filled 2ml syringe). However, this FHC would give acceptable test results as recently it has been reported that FHC of 100-351 IU/ml resulted in acceptable changes in pH, pCO2, pO2, Na+, K+, and Ca++ .Choice of blood:
Arterial blood specimens are the primary choice for BGA to assess ventilation and acid-base balance. However, arterial blood collection causes patient discomfort and other complications. Therefore, venous blood is often used for acid-base status assessment, although the composition of venous blood is influenced by the local activities of the organ drained by the vessel in question and the rate of blood flow through these peripheral tissues. It is thus not indicative of the acid-base status of the entire body. Moreover, opinions are divided on the use of venous blood over arterial blood. Central venous pH is usually 0.03 to 0.05 pH units lower than arterial blood pH, whereas peripheral venous pH is approximately 0.02–0.04 units lower. pCO2 is usually 4-5 mmHg higher in central venous blood, while in peripheral venous blood pCO2 is 3-8 mmHg higher than arterial pCO2. Regression equations have also been derived to estimate arterial values from venous values as follows: Arterial pH = -0.307 + 1.05 x venous pH Arterial pCO2 = 0.805 + 0.936 x venous pCO2 Arterial HCO3 = 0.513 + 0.945 x venous HCO3 However, a recent meta-analysis indicated that peripheral venous BGA compares well with arterial BGA for pH estimation in adults, but not for pCO2 or pO2. Nevertheless, venous percent oxygen saturation has been found to be a useful tool for treatment in sepsis. It is also crucial that the blood sample for BGA should be transported to the laboratory as quickly as possible because it should be analyzed for BGA within 15-30 minutes of blood collection. If there is any delay, then the syringe should be placed in ice-water slurry (not with ice alone) to reduce cellular metabolism. Steps for blood collection for BGA:- Take a small amount of heparin in a 2ml syringe to lubricate the inner wall of the syringe and then flush out the heparin completely.
- Collect 2ml arterial/venous blood in this heparinised syringe (filling the syringe completely is very important).
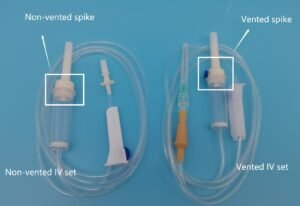
- Remove air bubbles quickly, if any, and place the needle cap (don’t bend the needle as it may hurt the analyst) or better, insert the tip of the needle into a rubber cap (of injection vial) or a bung to prevent any leakage of gases. Mix the blood in the syringe gently by rotating the syringe between the palms of the hands to ensure mixing of blood with heparin.
- Send the sample to the laboratory immediately. If it is not possible to send immediately, then keep the syringe in a container having ice-water slurry (not with ice alone), but not for too long because the plastic syringes are partially gas permeable, and this permeability increases at a lower temperature.
References
[1] Burnett RW, Covington AK, Fogh-Anderson N, Kulpmann WR, Maas AH, Muller-Plathe O, et al. International Federation of Clinical Chemistry (IFCC). Scientific division committee on pH, blood gases and electrolytes. Approved IFCC recommendations on whole blood sampling, transport and storage for simultaneous determination of pH, blood gases and electrolytes. Eur J Clin Chem Clin Biochem. 1995;33:247–53. [PubMed] [Google Scholar]
[2] Kune T, Sisman AR, Solak A, Tuglu B, Cinkooglu B, Coder C. The effects of different syringe volume needle size and sample volume on blood gas analysis in syringe washed with heparin. Biochemica Medica. 2012;22:189–201. [PMC free article] [PubMed] [Google Scholar]
[3] Hansen JE, Simmons DH. A systematic error in the determination of blood pCO2. Am Rev Respir Dis. 1977;115:1061–63. [PubMed] [Google Scholar]
[4] Hamilton RD, Crockett RJ, Alper JH. Arterial blood gas analysis: potential errors due to the addition of heparin. Anaesth Intensive Care. 1978;6:251–55. [PubMed] [Google Scholar]
[5] Bloom SA, Canzanella UJ, Strom JA, Madias NE. Spurious assessment of acid – base status due to dilutional effect of heparin. Am J Med. 1985;79:528–30. [PubMed] [Google Scholar]
[6] Adam AP, Hahn CEW. In: Principles and practice of blood-gas analysis. 2nd ed. Edinburgh Landon, Melbourne and New York: Churchil Livingstone; 1982. p. 64. [Google Scholar]
[7] Baird G. Preanalytical considerations in blood gas analysis. Biochemica Medica. 2013;23:19–27. [PMC free article] [PubMed] [Google Scholar]
[8] Milzma D, Jauchar T. In: Clinical procedures in emergency medicine, 4th Ed. Edited by Roberts JR, Hedges JR, Editors. Philadelphia: WB Saunders; 2004. Arterial puncture and cannulation; pp. 384–400. [Google Scholar]
[12] Byme AL, Bennett M, Chatterji R, Symons R, Pace NL, Thomas PS. Peripheral venous and arterial blood gas analysis in adults: Are they comparable? A systematic review and meta-analysis. Respirology. 2014;19:168–75. [PubMed] [Google Scholar]
[13] Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, et al. Surviving sepsis campaign: International guidelines for management of severe sepsis and septic shock. Crit Care Med. 2008;36:296–327. [PubMed] [Google Scholar]
[14] Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, et al. Early goal directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–77. [PubMed] [Google Scholar]